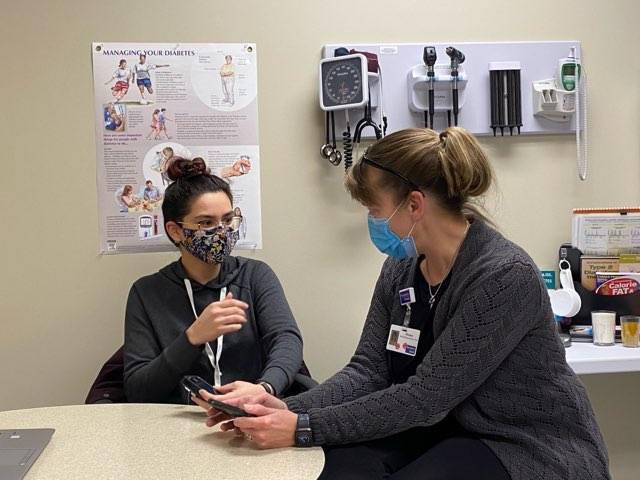
Diabetic Education Services

When you have concerns about diabetes, we're here to address those concerns –and any questions you have – with personalized care and the best information available. Our team of specialists works closely with your primary care provider to give you dependable support and the most advanced expertise to better manage your type-1 or type-2 diabetes diagnosis, along with any complications you may face.
Diabetic Support Services
You can rely on our dedicated Diabetes Management team to help better understand your condition and minimize its impact on your health and happiness, every day.
- Blood sugar, blood pressure and cholesterol monitoring
- Customized exercise programs
- Meal planning
- Medication and prescription support
- Treating diabetes-related symptoms and complications
Our Diabetic Management Clinic is conveniently located just south of Froedtert Kenosha Hospital in the Williams Building in the south parking lot (6334 8th Avenue, Kenosha).

Know Your Risk
Though a diabetes diagnosis can only be confirmed by a professional, the screening tests below can help determine if you or a loved one may be at risk for diabetes.
Our Doctors
Diabetic patients work directly with our board-certified endocrinologist, who brings extensive experience and an educational focus in helping patients manage their diagnosis and condition.


Location(s)
The signs and symptoms of diabetes can vary from person to person based on the level of glucose in the bloodstream at the time. Often, with prediabetes or early on with Type 2 diabetes symptoms go undetected. As glucose levels rise gradually the following symptoms may become noticed.
Early symptoms that may be overlooked
- Increased thirst
- Increased urination
- Feeling sweaty
- Increased hunger
- Weight loss
- Glucose in urine
- Ketones in urine- Usually associated with Type 1 diabetes (Ketones are a byproduct of the breakdown of fat as a result of too little insulin to utilize glucose for energy)
- Fatigue
- Frequent infections
- Slow wound healing
- Vision changes
- Mood changes, increased irritability
Late symptoms
- Sunken eyeballs
- Leg cramps
- Rapid breathing (Usually associated with Type 1 diabetes)
- Fruity breathing (Usually associated with Type 1 diabetes)
- Nausea & vomiting
- Unresponsiveness/coma
When to call the doctor and what to expect next
- If you notice any of the listed symptoms in yourself or your child, call your doctor.
- If you do not have a physician and are experiencing symptoms, go to your the walk-in clinic (mild symptoms) or emergency room (more severe symptoms). For assistance finding a physician call: 262-656-3627.
- The sooner the diagnosis is made, the less likely the affected person will be to experience severe, potentially life-threatening symptoms, that can occur if left undiagnosed.
Diabetes Mellitus refers to several diseases that affect the way our bodies utilize glucose for energy. Glucose is essential for our muscles and tissues survival in addition, it is the main source of energy for our brain.
Regardless of the type of diabetes, the common issue is: glucose levels increase in the blood stream and do not end up in the muscles & tissues as intended. They stay in the bloodstream and may accumulate to dangerous levels, causing damage if left uncontrolled.
Role of Glucose
We consume carbohydrates (various forms of sugar) in our diet, which digest and are referred to as glucose in our blood stream. Glucose is a source of energy for our muscles and the main source of energy for our brain.
Role of Insulin
Insulin is a hormone produced by the pancreas. When glucose levels in the bloodstream start to rise, insulin is secreted in response. It attaches to the receptors to the cells of muscles and tissues allowing glucose to enter and be utilized as energy. This results in glucose leaving the bloodstream (lowers blood glucose levels).
Type 1 diabetes
Type 1 diabetes used to be referred to as juvenile diabetes. Though type 1 can occur in the adult population as well, it is less common. Though the cause of type 1 diabetes is still unknown, it is believed that a combination of genetic susceptibility and environmental factors may contribute, though the environmental factors are still unknown.
What we do know is that type 1 diabetes is an autoimmune condition. The immune system usually fights off & destroys harmful bacteria & viruses by producing antibodies that protect us. With type 1 diabetes, the immune system instead attacks the beta cells of the pancreas that are responsible for producing insulin. This attack results in a near total to total loss of insulin production. Without insulin, glucose cannot enter the cells and will build up in the bloodstream.
Prediabetes and progression to type 2 diabetes
In prediabetes, the cells that utilize glucose for energy become resistant to insulin. Early on, the pancreas produces more and more insulin in an effort to compensate, but eventually cannot produce enough to overcome the resistance being met at the cell. This prevents glucose from getting into the cell, instead accumulating in the bloodstream.
If aggressive action & lifestyle measures are not taken during the prediabetes state, the disease will progress to type 2 diabetes, usually within 5-10 years.
It is believed that both genetic and environmental factors play a role in developing type 2 diabetes. Being overweight is also a risk factor, though not all people that develop prediabetes or type 2 diabetes are overweight.
Click below to take our screening test to see if you're at risk.
CDC Prediabetes Screening Test.pdf
Gestational diabetes
Gestational diabetes occurs during pregnancy. During pregnancy, the placenta produces hormones to maintain the pregnancy. These same hormones increase resistance to insulin at the cells. This results in higher glucose levels in the bloodstream. These increased blood glucose levels can be harmful to both mother and baby.
Normally, the pancreas can compensate and produce more insulin to account for the hormonal increases. When it cannot, gestational diabetes results. Women diagnosed with gestational diabetes are at greater risk for developing type 2 diabetes.
Risk factors for type 1 diabetes
- Family history: Parent or sibling with type 1 diabetes.
- Environmental factors: viral infection.
- Presence of diabetes autoantibodies: If you have a parent or sibling with type 1 diabetes, you may elect to be tested for diabetes autoantibodies. If you have these autoantibodies, your risk would be higher for developing type 1 diabetes.
- Dietary factors: vitamin D deficiency, early exposure to cow’s milk or cereals prior to age 4 months. *None have directly been proven to cause type 1 diabetes.
- Geography: Sweden & Finland have higher rates of type 1 diabetes than other countries throughout the world.
Risk factors for prediabetes and type 2 diabetes
- Weight: abdominal obesity and extra fatty tissue.
- Sedentary lifestyle/inactivity physical activity helps maintain weight & makes cells more sensitive to insulin.
- History of gestational diabetes. Having gestational diabetes increases your risk for type 2 later as well as having a baby weighing more than 9 pounds at birth.
- Race: African Americans, Hispanics, American Indians, and Asian Americans are all at greater risk for developing type 2 diabetes.
- Family history: If you have a parent or sibling with type 2 diabetes, your risk is increased.
- Polycystic ovary syndrome
- High blood pressure
- High cholesterol & triglyceride levels
Click below to take our Type 2 Diabetes risk test to find out if you are at risk.
Tests used to diagnose prediabetes and type 2 diabetes
- Hemaglobin A1c test
This test measures how much glucose is attached to the hemoglobin molecule of the red blood cell. Because the red blood cell lives about 3 months, this test gives a fair assessment of how your blood glucose level has averaged over a three month period of time.
A1c results
Normal: less than 5.4 mg/dl
Prediabetes: 5.5-6.4 mg/dl
Type 2 diabetes: greater than 6.5 mg/dl
- Fasting glucose test
This test is taken usually in the morning following an 8 hour period in which no food or caloric intake has been consumed.
Fasting blood glucose results
Normal: Less than 100 mg/dl
Prediabetes: 100-125 mg/dl
Type 2 diabetes: greater than 126 mg/dl
- OGTT: Oral glucose tolerance test
The patient is given a large glucose load and blood glucose level is measured 2 hours later. If the result is greater than 200 mg/dl, the result is indicative of type 2 diabetes.
- Random blood glucose
If a finger stick performed at any time is greater than 200 mg/dl, it is diagnostic for being type-2 diabetic.
Tests used to diagnose Type 1 diabetes
Any of the above tests in addition to antibody testing. If a patient has an autoantibody associated with type 1 diabetes, this confirms the diagnosis.
- C-Peptide
This test measures how much C-peptide is in your blood. Because levels of this peptide generally match insulin levels in the body, the test can indicate how much insulin your body is producing. Low levels of C-peptide and insulin usually point to type 1 diabetes. However, low C-peptide levels can be found in patients that have had type 2 diabetes for years and have become dependent on insulin.
- Glutamic Acid Decarboxylase Autoantibodies (GADA or Anti-GAD)
This test seeks to find antibodies built against a specific enzyme in the pancreatic beta cells that produce insulin.
- Insulin Autoantibodies (IAA)
In addition to attacking beta cells, the immune system also targets insulin in people with type 1 diabetes. This test looks for the antibodies targeting insulin.
- Insulinoma-Associated-2 Autoantibodies (IA-2A)
This test looks for antibodies mounted against a specific enzyme in beta cells. Both the IA-2A and GADA tests are common type 1 antibody tests performed at endocrinology offices.
Prediabetes & Type 2 diabetes
- Medication
- Diet & exercise (all types of diabetes)
- Oral agents
- Non-insulin injectables
- Insulin
- Diabetes self-management education
- Learn self-management skills, such as monitoring blood glucose levels, healthy lifestyle habits (diet, exercise, meal planning), medication management, troubleshooting blood glucose readings and balancing with medication, how to manage hypoglycemia and hyperglycemia, proper foot care, complication prevention skills, stress management, sick day management and risk reduction skills.
The treatment options above may be used together in many cases.
Type 1 diabetes
- Multiple daily dose injections of insulin or insulin pump therapy.
- Learn self-management skills, such as monitoring blood glucose levels, healthy lifestyle habits (diet, exercise, meal planning), medication management, troubleshooting blood glucose readings and balancing with medication, how to manage hypoglycemia and hyperglycemia, proper foot care, complication prevention skills, stress management, sick day management and risk reduction skills.
Resources
For more information about managing diabetes, we encourage you to explore any of the following resources.
The American Diabetes Association is a network of diabetes patients, medical professionals and patient advocates who work to prevent and cure diabetes and to improve the lives of all people affected by diabetes. Our clinic is certified by the American Diabetes Association, meaning that you can count on receiving the most up to date information and guidance in managing your condition.
The Juvenile Diabetes Association is the leading global organization funding type-1 diabetes (T1D) research. Its mission is to improve lives, today and tomorrow, by accelerating life-changing breakthroughs to cure, prevent and treat T1D and its complications.
The U.S Department of Health and Human Services runs the National Institute of Diabetes and Digestive and Kidney Diseases, which provides a number of resources and diabetes-related information for whose lives have been affected by a diabetes diagnosis.
Phone Numbers
-
Diabetic Education
262.656.2597
Diabetic Education Services
Successfully treating or managing diabetes requires support. You can rely on our full diabetes management team to work closely with you and your family physician, ensuring comprehensive care for patients of all ages throughout our community.


